Shweta Mittal1, Saurabh Bansal2
1 Department of Otorhinolaryngology, Nirmal Hospital, Rishikesh, Uttarakhand, India
2 Department of Radiation Oncology, Cancer Research Institute, SRHU, Dehradun, Uttarakhand, India
| Date of Submission | 30-Mar-2020 |
| Date of Decision | 17-Apr-2020 |
| Date of Acceptance | 17-May-2020 |
| Date of Web Publication | 06-Aug-2020 |
Correspondence Address:
Dr. Saurabh Bansal
Department of Radiation Oncology, Cancer Research Institute, SRHU, Dehradun, Uttarakhand
India
Source of Support: None, Conflict of Interest: None
DOI: 10.4103/jcar.JCar_7_20
Abstract
INTRODUCTION: The behavior of the laryngeal squamous cell carcinoma (LSCC) is marked by the degree of cell proliferation and differentiation. Ki-67 is regarded as a promising proliferation marker and has been correlated as a prognostic indicator.
AIM: The aim of the present study is to determine the Ki-67 expression and its prognostic value in LSCC.
MATERIALS AND METHODS: A total of eighty patients with early glottic carcinoma stage (Tis, T1, T2) N0M0were included. After preoperative workup, surgery was performed using LUMINES 40C CO2laser and tumor resection was done which was sent for histopathological diagnosis and immunohistochemistry (IHC). IHC for Ki-67 expression could be done only on 65 specimens.
RESULTS: All patients had microscopically confirmed squamous cell carcinoma. Forty-eight out of 65 specimens (75%) stained positive for Ki-67 and 17 (25%) stained negative. Out of total 48, 29 stained 2+, 11 stained 3+ and 8 stained 4+. No difference was found in Ki-67 expression in relation to age, sex, T stage, and histological grading. The association of Ki-67 with recurrence was found to be statistically significant. The association of Ki-67 with survival was also studied and Ki-67 positivity is associated with increased mortality rate, although it was not statistically significant.
CONCLUSION: The proliferative index as measured by immunohistochemical staining of Ki-67 correlates with the tumor aggressiveness. High Ki-67 index is associated with early relapse and poor survival outcomes.
Keywords: Immunohistochemistry, Ki-67, proliferation, squamous cell carcinoma
| How to cite this article: Mittal S, Bansal S. Expression of Ki-67 in early glottic carcinoma and its relation to oncological outcomes following CO2laser microsurgery. J Carcinog 2020;19:7 |
| How to cite this URL: Mittal S, Bansal S. Expression of Ki-67 in early glottic carcinoma and its relation to oncological outcomes following CO2laser microsurgery. J Carcinog [serial online] 2020 [cited 2021 Oct 15];19:7. Available from: https://carcinogenesis.com/text.asp?2020/19/1/7/291579 |
Introduction
Laryngeal carcinoma is the second most common head and neck cancer worldwide[1] and about 90% of these cases are squamous cell carcinomas (SCCs).[2] The incidence is high in India because of certain habits such as oral intake of tobacco, betel nut, and pan masala chewing.[3] Of the sites in larynx, glottis is the most commonly affected site (50%). Glottic cancer presents with change in voice/hoarseness and thus can be detected early. Treatment planning generally requires a multidisciplinary approach and selection of appropriate treatment depends on tumor site, extent of tumor, patient nutritional status, concomitant health problems, social and logistic factors, and patient preference.
Identification of biomarkers that can detect cancer early, monitor disease progression, or serve as a surrogate marker for prognosis will enable to personalize treatment and improve care of cancer patients. The behavior of the SCC is marked by the degree of cell proliferation and differentiation, and this index can be derived by measuring Ki-67.[4],[5] The Ki-67, which is a nuclear antigen present only in the nuclei of cycling cells, is a tumor growth marker and can be readily detected using immunohistochemistry (IHC) methods. It is a potential prognostic biomarker in a variety of tumors, including laryngeal neoplasms.[6]
Historically, the definite treatment for laryngeal carcinomas has been open surgery to excise the tumor en bloc with negative microscopic margins. However, despite providing good oncological control, open laryngectomies have detrimental impact on quality of life. Transoral laser microsurgery is an emerging technique and is increasingly being used in place of traditional open surgery because of lower morbidity and improved organ preservation. Currently, treatment options for early glottic malignancies include radiotherapy (RT), transoral CO2 laser excision, and vocal cord stripping, with cordectomy and partial laryngectomy reserved for salvage therapy.
Many studies have been conducted relating Ki-67 to oncological outcomes following RT but only few has been done following CO2 laser microsurgery.[7] These studies found that an increase in Ki-67 index resulted in greater risk of recurrence and also reinforced the role of Ki-67 as a marker of tumor aggressiveness in laryngeal squamous cell carcinoma (LSCC).
The aim of this study is to discuss and summarize the results obtained so far as to the proliferative activity of early glottis tumors, in an effort to verify if cell proliferation can really provide useful prognostic information in these tumors or not.
Materials and Methods
Patient selection
This prospective study was undertaken in Department of Otorhinolaryngology and Department of Pathology at University College of Medical Sciences and GTB Hospital from November 2011 to April 2015. Total of eighty cases were taken after taking written informed consent and ethical clearance certificate from Institutional Ethics Committee. All cases were staged as per the AJCC tumor-node-metastasis (TNM) 2002 staging system. IHC for Ki-67 expression could only be done on 65 specimens. Inclusion criteria was patients of early glottic carcinoma stage (Tis, T1, T2) N0M0. Any patient with the history of previous RT or laryngeal surgery, history of previous malignancy of head and neck, any supraglottic pathology obscuring stroboscopic view, cases with recurrent disease, or unavailability of adequate tissue were not included in the study. Preoperative evaluation includes complete history and physical examination (general and local), indirect laryngoscopy, videolaryngostroboscopy (VLS), and computed tomography/magnetic resonance imaging if required to exclude cartilage invasion.
Treatment
After preoperative workup, surgery was performed under general anesthesia using LUMINES 40°C CO2 laser with superpulse continuous mode coupled with acuspot micromanipulator and tumor resection was done which was sent for histopathological diagnosis and IHC. After histopathological confirmation of SCC, 5 tissue microarrays were constructed manually. 3–4 μm thick sections were taken from each microarray block for hematoxylin and eosin staining and Ki-67 immunohistochemical staining. For IHC demonstration of Ki-67, sections were deparaffinized and rehydrated. Antigen retrieval was done by heating in EZ Retriever System V.2.1 from BioGenex for two cycles of 10 min at 95°C in citrate buffer (pH 6.0). Endogenous peroxidases were blocked by 4% H2O2 for 30 min followed by 3 washings of 5 min each with tris(hydroxymethyl)aminomethane (TRIS) buffer. The sections were incubated with the monoclonal anti-Ki-67 (rabbit monoclonal anti-Ki-67, clone SP6 from Biocare Medical) in 1:100 dilution. The slides were then incubated overnight at 4°C and the next morning, three washes with TRIS buffer were given. Blocking solution was then blotted off without rinsing and mouse-anti-digoxigenin was applied. Again, the slides were washed in phosphate buffer saline before applying diaminobenzidine solution for development of color and were counter stained with Mayer’s hematoxylin. Slides were then dehydrated, cleared, and mounted using alcoholic mounting solution.
Immunohistochemistry scoring system
The slides were examined at ×400 magnification. Amount of positive staining cells were assessed as the estimated percentage of positive staining cells. (0/1+ = negative/low, 2+/3+/4+ = positive/high) [Figure 1], [Figure 2], [Figure 3]:
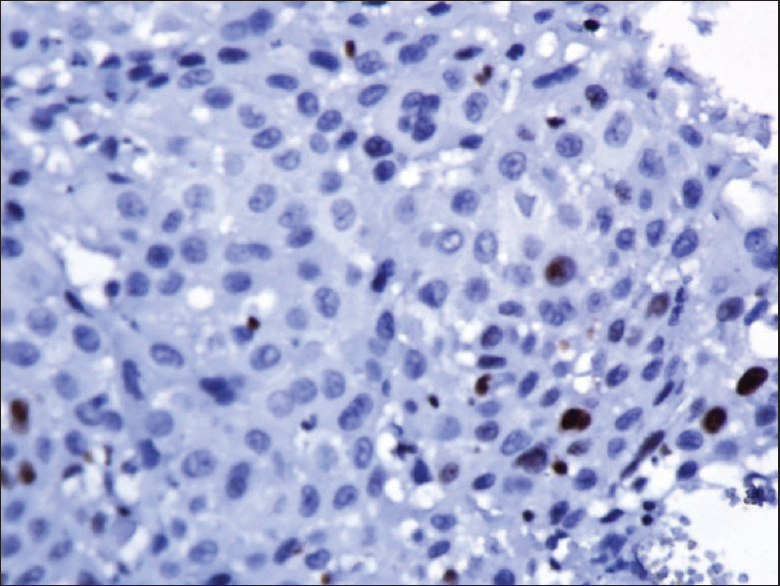 |
Figure 1: Immunohistochemistry ×400 showing Ki 67 staining in less than 10% of cells (1+) Click here to view |
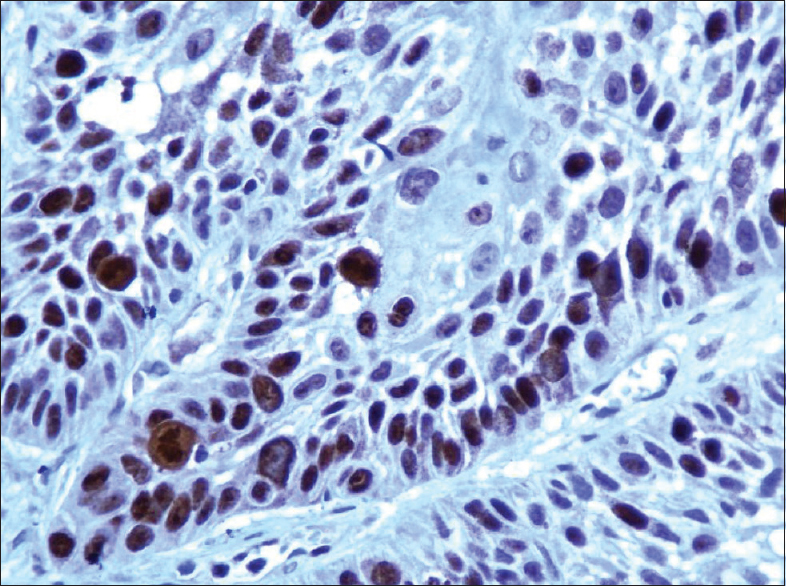 |
Figure 2: Immunohistochemistry ×400 showing Ki 67 staining in 10%–50% of cells (2+) Click here to view |
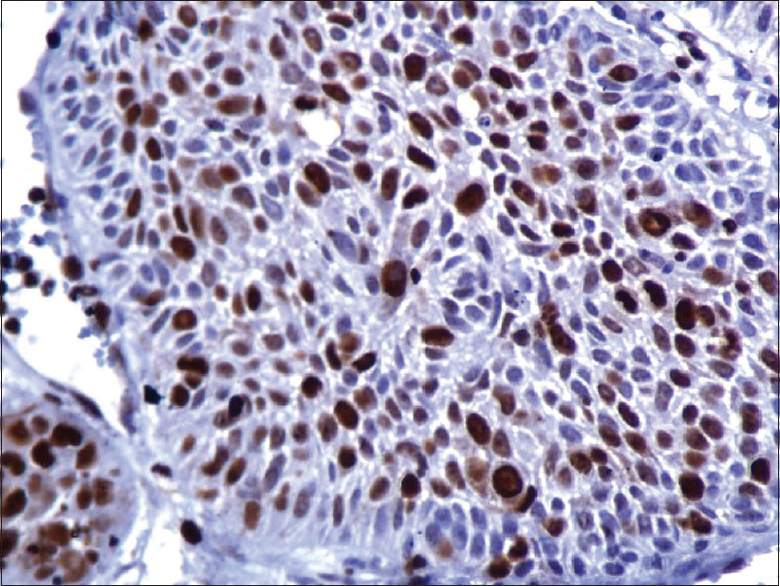 |
Figure 3: Immunohistochemistry ×400 showing Ki 67 staining in more than 75% of cells (4+) Click here to view |
- 0 – 0% staining
- 1+ – <10% staining
- 2+ – 10-50% staining
- 3+ – 50-75% staining
- 4+ – >75% staining.
Follow-up
Each patient was followed up every 3 months in 1st year and every 6 months thereafter with minimum follow-up of 6 months. On each follow-up visit, patients were assessed for: General physical examination, VLS, and recurrence-local/regional. Oncological outcomes were assessed in terms of local and regional recurrence.
Data management and statistical analysis
- Interpretation and analysis of obtained results were carried out using software IBM SPSS Statistics for Windows, version 22 (IBM Corp., Armonk, N.Y., USA by application of descriptive methods (mean, rate, ratio, proportional, etc.,). Categorical variables were expressed as frequencies and percentages.
Results
A total of eighty patients were included in the present study with mean age 58.9 years (range 27–78 years). Subjects were predominantly male with a male:female ratio of 15:1. Most of the patients were in T1a stage. Summary of the baseline characteristics is shown in [Table 1]. The most common symptom was hoarseness ranging in duration from 3 months to 12 months followed by throat pain, decreased appetite, coughing, and fatigue. The most commonly associated addiction was smoking which was seen in 95% of patients. The mean follow-up of all patients was 24.31 months (6–53 months).
| Table 1: Summary of the baseline characteristics Click here to view |
Surgical excisions were tailor-made as per the extent of the tumor guided by microscopic evaluation and laser-tumor interaction as shown in [Graph 1]. Maximum numbers of patients were treated by Type III cordectomy (29%).
The tissue obtained after surgery using CO2 laser was subjected to histopathology. All patients had microscopically confirmed SCC. Of these, 16 (20%) patients had carcinoma in situ [Grade 1], 21 (27%) had well differentiated [Grade 2] and 43 (53%) had moderately differentiated [Grade 3]. All the patients had documented negative margins and were put on follow-up as per the study protocol.
Over follow-up for entire cohort of eighty cases, eight patients were lost to follow-up. The mean follow-up of all patients was 24.31 months (4–53 months). Twenty cases (25%) developed local recurrence within periods varying from 4 to 19 months (mean 11.38 months). Out of these twenty patients, eight patients were offered rescue treatment in form of repeat endoscopic CO2 laser cordectomy, five patients underwent total laryngectomy, three patients were directly referred for RT, two patients refused for further treatment, two patients died of unrelated causes before they could be subjected to another treatment.
Out of eight patients who were given rescue treatment in form of repeat endoscopic CO2 laser cordectomy two patients received RT. Three out of five patients who underwent total laryngectomy died due to carcinoma at 12, 24 and 28 months.
Remaining 55 patients and 5 patients who had repeat endoscopic resection (at recurrence) were disease free at the end of the study period and retaining good physiological functions of voice and tracheostomy free airway. Out of these sixty patients five patients died of natural causes after 1 year of surgery.
The specimens were subjected to IHC for detection of Ki-67 antigen and analysed according to patient and tumour related characteristics as shown in [Table 2].
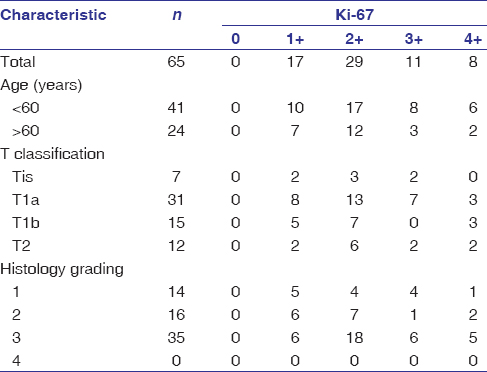 |
Table 2: Ki-67 distribution according to patient and tumor-related characteristics in 65 patients and analysis Click here to view |
Number of cells staining positive for anti-Ki-67 antibodies were looked for and graded as percentage of total cells. Out of 80 specimens, Ki-67 antibodies could be applied to 65 specimens as some specimens were too little and were lost during processing and were excluded. 48 out of 65 specimen (75%) stained positive for Ki-67 and 17 (25%) stained negative. Out of total 48, 29 stained 2+, 11 stained 3+, and 8 stained 4+.
No difference was found in Ki-67 expression in relation to age, sex, T stage and histological grading. The association of Ki-67 with recurrence was studied. First, Ki-67 was taken as nominal variable like negative or positive and Fisher’s exact test was applied. The relationship was found significant (P = 0.049) as shown in [Table 3]. Than Ki-67 was also taken as ordinal variable 1+, 2+, 3+, 4+ and Pearson’s Chi-square test was applied. This relationship was again found to be significant (P = 0.005) as shown in [Table 4].
| Table 3: Analysis of Ki-67 with recurrence using Ki-67 as nominal variable Click here to view |
| Table 4: Analysis of Ki-67 with recurrence using Ki-67 as ordinal variable Click here to view |
Survival analysis
Survival curves were computed through Kaplan–Meier method. Out of total eighty patients, nine patients died due to causes unrelated to Ca larynx and were not included in the analysis. One-year, 2-year, and 3-year overall survival rates were calculated and were 96.5%, 94.2%, and 91.2%, respectively.
Survival rates were calculated using Ki-67 first as nominal variable and then as ordinal variable as shown in [Graph 2] and [Graph 3].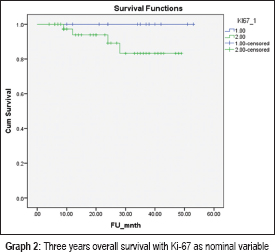
Above data indicate that Ki-67 positivity is associated with increased mortality rate, although it was not statistically significant.
Above data indicate that higher Ki-67 positivity is associated with increased mortality rates.
Discussion
Squamous cell carcinoma of the larynx (SCCL) is the most common malignancy in the head and neck region. The combination of surgical or laser-surgical resection and/or chemoirradiation is considered as state of the art in the treatment of these tumors.[8] It still is difficult to give an exact prognosis for the clinical course of SCCL with the established clinical parameters such as the TNM classification and the histopathological grading.[9] In order to establish the prognostic factors, it is important to understand the biologic evolution and the natural history of laryngeal cancer.
High proliferation rate of the tumor cells correlates with aggressive clinical course and tendency to metastasize early. This indicates that proliferation index might be an important factor for prognosis and therefore proliferation markers may help determine treatment outcomes and may influence therapy indications.[10]
Cell cycle proteins, Ki-67 and p100, had been extensively studied to determine the proliferative activity of normal or neoplastic cell populations. Ki-67 is expressed in all active phases of the cell cycle except the G0-phase and is nowadays seen as the most reliable proliferation marker.[4],[5] Our study was to evaluate expression of Ki-67 in early glottic carcinoma and its relation to oncological outcomes following CO2 laser microsurgery.
In the present study, no difference was found in Ki-67 expression in relation to age, sex, T stage, histological grade, and anterior commissure involvement. The P value in these parameters was found to be >0.05. However, Acikalin et al.[11] studied 63 patients with LSCC and reported a significant correlation between Ki-67 index and patient age, tumor stage. There was no significant association between the Ki-67 mean proliferation index and tumor site or histologic grade.
The role of Ki-67 as a prognostic marker for and survival has been evaluated in many studies in various cancers including laryngeal tumors; however, contradictory results have been published.
In our study, the association of Ki-67 with recurrence was studied taking it as both nominal (P = 0.049) and ordinal variable (P = 0.005) and the results were found to be statistically significant indicating that Ki-67 positivity is a strong predictor for early relapse.
Sittel et al.[7] and Fumic-Dunkic et al.[12] in their respective studies analyzed that the Ki-67 labeling index was significantly (P = 0.01) higher in tumors from patients who had treatment failure. They concluded that high Ki-67 may be associated with early relapse of laryngeal carcinoma treated with transoral laser surgery and could be used as a predictive marker for assessing the course, prognosis, and treatment success in carcinoma larynx.
Lazaris et al.,[13] in 2002, studied relapse-free survival in 96 patients of SCC larynx with positive Ki-67 nuclei. There was a statistically significant association between Ki-67 immunopositivity index >20% and relapse (P > 0.0005). They found that high Ki-67 index resulted in greater risk of recurrence and also reinforced the role of Ki-67 as a marker of aggressiveness in laryngeal carcinoma.
The immunohistochemical assessment of Ki-67 is an important prognostic indicator and studies[12],[13] have shown that tumors with high proliferation indices are less favorable in terms of survival, but others[14] did not find any relation. Reasons for these discordant results may include the selection of heterogeneous tumors in terms of stage and site, the small number of cases studied, the differences in proliferation markers and in evaluation methods.
In the present study, the association of Ki-67 with survival was studied taking it as both nominal (P = 0.049) and ordinal variable (P = 0.005) and Ki-67 positivity was associated with increased mortality rate indicating that Ki-67 positivity is a strong predictor for poor survival, although it was not statistically significant. In a study done by Re et al.[15] in 2014, Ki-67 immunostaining was found to be a major determinant in tumor cell survival for LSCC. Their findings support the hypothesis that quantitative assessment of Ki-67 may be useful in predicting prognosis and clinical outcome in LSCC.
Acikalin et al.[11] in their study on 63 laryngeal SCC reported a significant correlation between Ki-67 mean proliferation index and T-stage (P < 0.05), nodal metastasis (P = 0.001), and recurrence (P < 0.001). Moreover, Kaplan–Meier plots of survival showed that a high Ki-67 labeling index correlated with a shorter disease-free survival (P < 0.0001).
Cordes et al.[16] analyzed the proliferative activity of 104 SCCs of the larynx detecting the Ki-67 antigen. The patients with low proliferating laryngeal cancers had a statistically longer recurrence-free 5-year survival time than patients with a highly proliferating cancer (P < 0.05). Also, the patients with low Ki-67 had a better 5-year overall survival rate of 84%, compared to patients with a high Ki-67 47.18% (P < 0.05).
Conclusion
Given these findings, we believe that that high proliferative index (Ki-67) correlates with aggressive clinical course and worse prognosis in patients affected by LSCC. However, further randomized studies with large sample size and longer follow-up are required to establish Ki-67 as a definitive predictive and prognostic marker in early stage glottis cancers.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
| 1. | |
| 2. | |
| 3. | |
| 4. | |
| 5. |
Ashraf MJ, Maghbul M, Azarpira N, Khademi B. Expression of Ki67 and P53 in primary squamous cell carcinoma of the larynx. Indian J Pathol Microbiol 2010;53:661-5.
 [PUBMED] [Full text] |
| 6. | |
| 7. | |
| 8. | |
| 9. | |
| 10. | |
| 11. | |
| 12. | |
| 13. | |
| 14. | |
| 15. | |
| 16. |
